
Trigeminal neuralgia (TN) is a long-term pain condition impacting the trigeminal nerve, one of the most extensive nerves in the head. Known for causing severe, sporadic, and often debilitating facial pain, TN can greatly reduce the quality of life. While the exact cause of TN isn’t always known, there’s increasing interest in its hereditary aspects. This article delves into whether trigeminal neuralgia can be inherited and how a family history might affect the likelihood of developing this painful disorder.
Understanding Trigeminal Neuralgia
Trigeminal neuralgia, also known as tic douloureux, is a nerve disorder causing intense, stabbing facial pain. Simple activities like chewing, speaking, or even touching the face can trigger this pain. There are two main types of TN:
- TN1 (Classic Trigeminal Neuralgia): Sudden, severe, shock-like pain.
- TN2 (Atypical Trigeminal Neuralgia): Persistent aching, burning, or stabbing pain that is less intense but more constant than TN1.
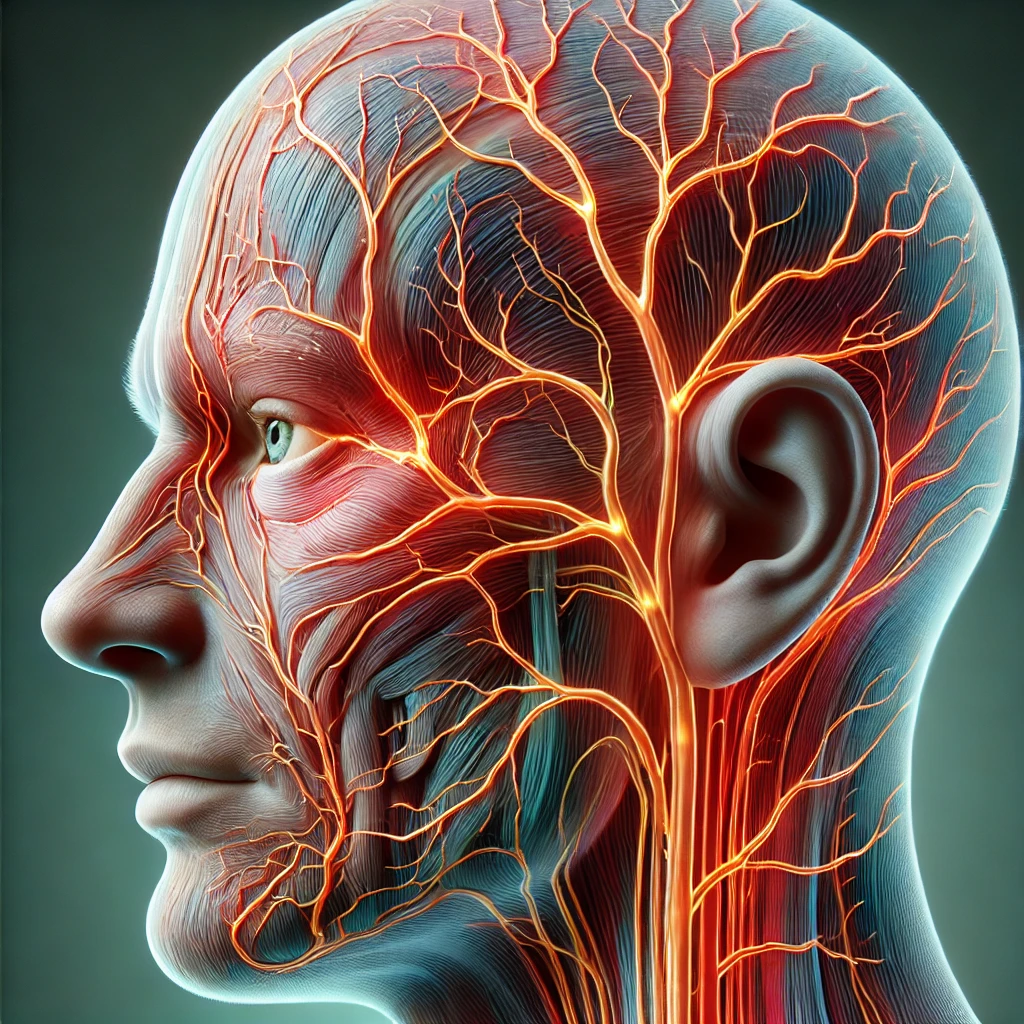
The Trigeminal Nerve
The trigeminal nerve is the fifth cranial nerve, responsible for facial sensation and some motor functions like biting and chewing. It has three branches:
- Ophthalmic branch: Sensation to the forehead and eyes.
- Maxillary branch: Sensation to the cheeks and upper lip.
- Mandibular branch: Sensation to the jaw and lower lip, also controls some chewing muscles.
Diagnosis and Treatment
Diagnosing TN involves clinical evaluation, medical history, and imaging tests like MRI to rule out other causes. Treatment options include medications like anticonvulsants and antispasmodics, and surgical interventions such as microvascular decompression and gamma knife radiosurgery.
Causes of Trigeminal Neuralgia Primary vs. Secondary TN
TN can be primary (idiopathic) or secondary (caused by another condition). Primary TN has no clear cause, while secondary TN results from conditions like multiple sclerosis or tumors compressing the trigeminal nerve.
Potential Triggers
Several factors can trigger TN, including:
- Blood vessel compression: A blood vessel pressing on the trigeminal nerve, leading to demyelination and pain.
- Multiple sclerosis: TN can occur in people with multiple sclerosis due to nerve fiber demyelination in the brain and spinal cord.
- Other underlying conditions: Tumors, cysts, or other structural abnormalities can also cause TN.
Hereditary Aspects of Trigeminal Neuralgia Genetic Predisposition
Increasing evidence suggests genetic factors may play a role in TN. Although not purely hereditary, having a family member with TN can increase the risk. Studies show familial patterns of TN, indicating genetics may influence susceptibility.
Family History
Research indicates individuals with a family history of TN are more likely to develop the condition. A study in “Neurology” found first-degree relatives of TN patients have a higher risk compared to the general population, suggesting a genetic predisposition.
Specific Genes Involved
Current research explores specific genetic markers linked to TN. While no single gene is definitively connected to TN, several genes involved in nerve function and pain pathways are under investigation. Understanding these genetic factors could lead to better diagnostics and treatments.
Familial Risk Factors and Trigeminal Neuralgia Inherited Traits
Genetics can affect TN susceptibility, including nerve compression and pain response. Individuals with a genetic predisposition may have nervous system structural differences making them more prone to TN.
Epigenetics
Epigenetic factors, involving changes in gene expression rather than genetic code, also play a role. Environmental factors like stress, diet, and toxin exposure can influence gene expression related to TN, potentially triggering symptoms in genetically predisposed individuals.
Managing Trigeminal Neuralgia with a Family History Early Detection
Early detection is crucial for families with a history of TN. Recognizing early signs and symptoms can lead to prompt diagnosis and treatment, potentially preventing the condition from worsening.
Genetic Counseling
Genetic counseling benefits individuals with a family history of TN. Genetic counselors can assess the risk based on family history and guide preventive measures and early intervention strategies.
Preventive Measures and Lifestyle Changes
While TN may not be entirely preventable, certain lifestyle changes can help manage the condition and reduce trigger episodes:
- Diet: Maintaining a healthy diet and avoiding triggers like caffeine and alcohol can help manage symptoms.
- Stress Management: Stress can trigger TN episodes. Techniques like mindfulness, meditation, and yoga can reduce stress.
- Regular Exercise: Physical activity improves overall health and helps manage stress, potentially reducing TN attacks’ frequency and severity.
Advances in Research and Future Directions Current Studies
Ongoing research focuses on identifying genetic markers and understanding TN’s hereditary aspects. Studies explore specific genes in nerve function and pain perception, potentially leading to more targeted treatments.
Potential Treatments Targeting Genetic Causes
Future TN treatments may include therapies targeting specific genetic factors. Gene therapy could correct genetic defects contributing to TN, offering a more effective and personalized approach.
The Role of Personalized Medicine
Personalized medicine, tailoring treatment to an individual’s genetic profile, shows promise for TN patients. Understanding genetic factors can help healthcare providers develop more effective treatment plans addressing the condition’s underlying causes.
Conclusion
In conclusion, while trigeminal neuralgia isn’t purely hereditary, family history and genetic factors can influence the likelihood of developing the condition. Understanding TN’s hereditary aspects can help individuals with a family history manage their risk. Early detection, genetic counseling, and lifestyle changes are crucial in managing TN and improving life quality for those affected. As research uncovers genetic factors, personalized medicine may offer new and more effective TN treatments in the future.
References
- Zakrzewska, J. M., & Linskey, M. E. (2014). Trigeminal neuralgia. BMJ, 348, g474.
- Katusic, S., Beard, C. M., Bergstralh, E. J., Kurland, L. T. (1990).
- Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945-1984.
- Annals of Neurology, 27(1), 89-95.
- Di Stefano, G., Truini, A. (2017). Pharmacological treatment of trigeminal neuralgia. Expert Review of Neurotherapeutics, 17(10), 1013-1021.






